|
www.HealthyHearing.com |
All about: Over-the-counter hearing aidsHow to know if OTC devices are right for you
Contributed by Emily Ostrowski, content manager, Healthy Hearing In October 2022 the FDA approved over-the-counter hearing aids for mild to moderate hearing loss in adults, with the stated goal of making hearing care more affordable and accessible. 
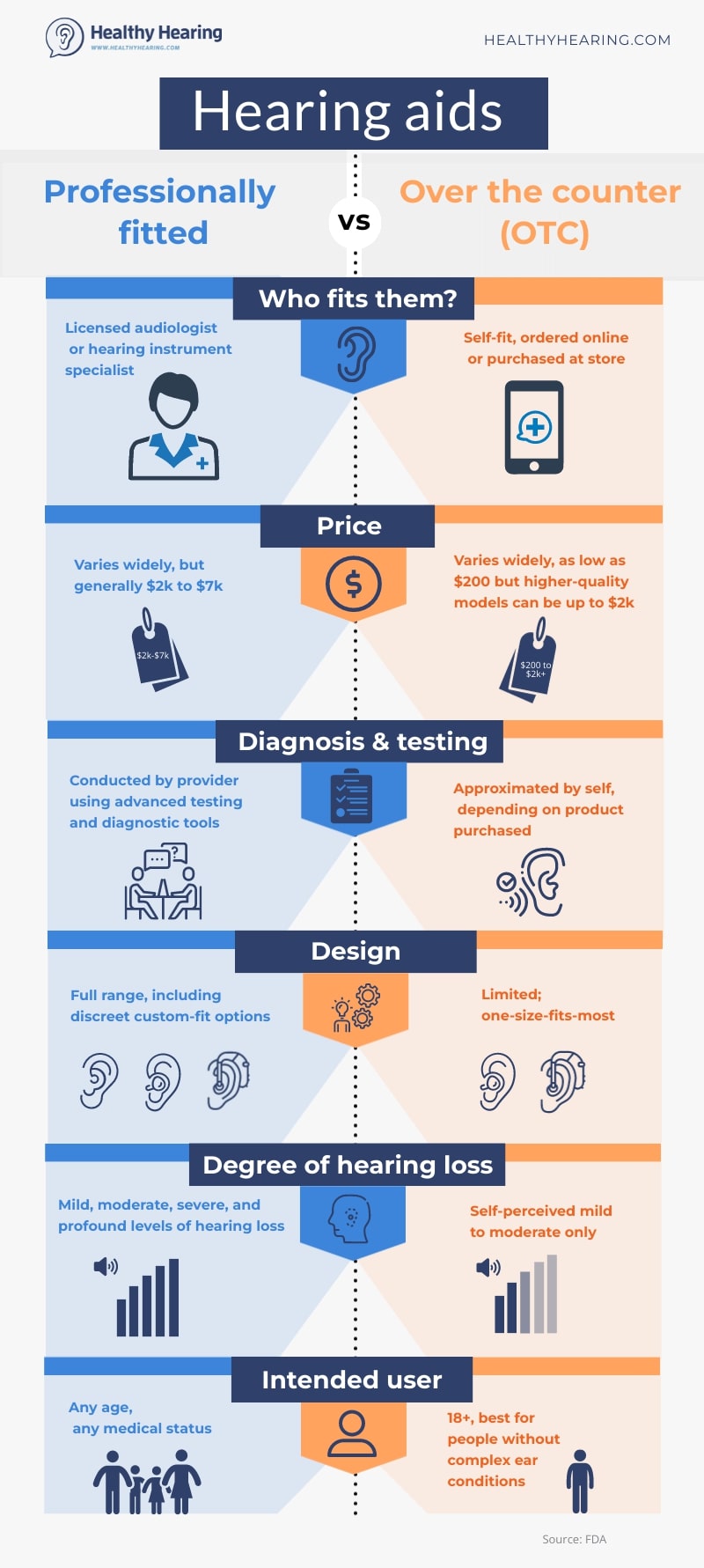
However, more than two years later, many people are still confused about how OTC hearing aids work and if they are the best choice for them. With that in mind, let's take a look at common questions people have, and key pros and cons to keep in mind. How are OTC hearing aids different than prescription hearing aids?Perhaps the two biggest questions are 1) how do OTC hearing aids differ from prescription or professionally-fitted hearing aids and 2) do they work as well? To the first question, OTC and prescription hearing aids differ in several key ways:
Types of hearing loss treatedOver-the-counter hearing aids are only intended for adults with mild to moderate hearing loss. They are not meant for children or people with more severe or profound hearing loss, both of which can be treated with prescription hearing aids. OTC hearing aids should also never be used if you experience sudden hearing loss in one or both ears. If you experience a sudden change in hearing, seek medical attention right away to get proper treatment. Want to learn more? Check out our in-depth piece on who should not get OTC hearing aids. Initial visit and testingThe most obvious difference is that you don't need a hearing test or fitting by an audiologist or hearing professional to purchase OTC hearing aids. While getting a professional hearing test is the best way to determine what type of hearing loss you have, factors like the cost of care, lack of insurance coverage or minimal to no accessibility to a hearing specialist can make OTC options easier to obtain. It's important to note that even though you don't need a hearing test to get OTC hearing aids, you can use your results from a professional test to help determine if they are right for you. The results can also help you when you self-fit and select your settings. CostIn general, the cost of a pair of OTC hearing aids is less than a professionally-fitted pair. The least expensive options can cost as little as $200. However more premium (and often more effective) models can be similar in price to prescription hearing aids, running between $1,500-2,000. Customization and stylesOver-the-counter hearing aids don't have as many options for customization. Styles are comparatively limited and more "one size fits all." While some OTC brands come with features like Bluetooth, none currently offer telecoil, a popular feature that allows users to hear better in public places with hearing loops. Additionally, OTC hearing aids do not offer custom earmolds, which are needed for a secure, comfortable fit and optimal sound quality—especially for those with small or uniquely shaped ear canals. Hearing care before and afterAudiologists do more than conduct comprehensive hearing evaluations before fitting patients with prescription hearing aids. They also:
On the other hand, while some OTC models include apps, tech support, and the ability to ask questions from hearing specialists, the guidance is limited and lacks in-person, real-time adjustments. 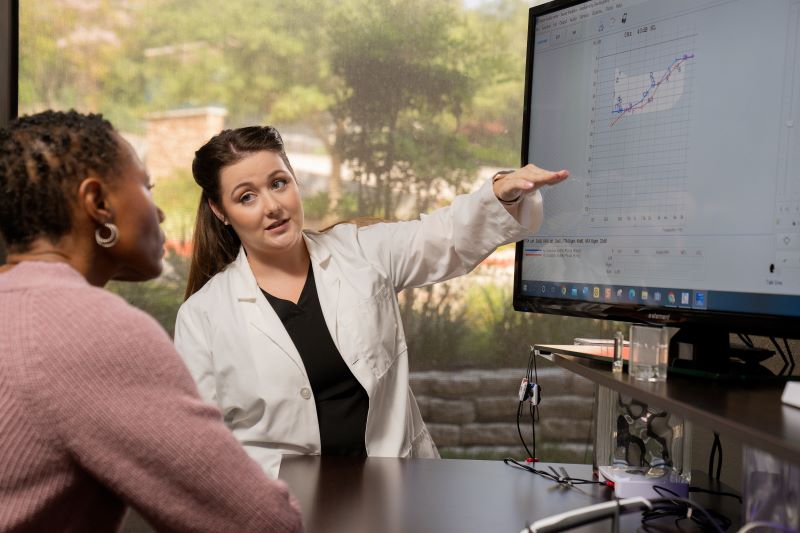
provide in-depth hearing care, including education. As Juliëtte Sterkens, audiologist and hearing loop advocate for the Hearing Loss Association of America (HLAA) notes, "Since the user is on his or her own, people must be a bit tech-savvy." People who are comfortable with downloading apps and updating their phone software may have no problem with self-fitting, but others may struggle without hands-on assistance. What users are sayingA 2023 survey on OTC hearing aids from the American-Speech-Language-Hearing Association (ASHA) found that nearly half of all users who purchased over-the-counter devices were highly satisfied. However, the majority of respondents felt that it was important for prospective users to receive professional guidance before purchase. Users in popular Reddit forums r/HearingAids and r/hardofhearing have expressed a variety of opinions on OTC versus professionally fitted hearing aids, as well. One user bought an OTC pair after his wife expressed satisfaction with hers and appreciates that they have features that allow him to stream music and take phone calls while using them. Another person chimed in that they bought an OTC pair after having prescription hearing aids for awhile. "When my prescription hearing aids broke I decided to try a pair of OTC instead. They are similar in their performance, but not as much fine tuning as a prescription pair." Others have similarly appreciated the professional care they get with prescription options. "I was seriously considering some OTC options, but now having gone to an audiologist and talking about my results and what he's going to do in terms of 'fitting,' I'm glad I'm not going OTC. I might feel more comfortable going OTC in the future, but as a newbie I'm appreciating the expert assistance." Even an audiologist chimed in saying that while some kind of amplification is better than nothing and OTC hearing aids make hearing help more accessible, expectations should be realistic—they offer only limited benefit and don't cater to a person's individual degree of hearing loss at each frequency. So, do they work as well?In a nutshell: OTC devices in general are not going to provide the same quality of hearing as professionally-fitted devices. However, adults with mild to moderate hearing loss who are comfortable with self-fitting and managing their own device settings may find them a helpful and worthwhile investment. Where do I get an OTC hearing aid?Over-the-counter hearing aids are available in multiple places, such as:
Some traditional hearing aid clinics also sell OTC options, but they typically focus on professionally-fitted options. Can AirPods be OTC hearing aids?Yes. In September 2024, the FDA authorized Apple's Hearing Aid Feature software for over-the-counter (OTC) use with AirPods Pro 2. This feature became available with the iOS 18 update, allowing the earbuds to function in many of the same ways as OTC hearing aids. The software also performs a hearing test to better gauge the user's hearing profile. In September of 2025, Apple introduced AirPods Pro 3, which continue, and in some ways improve upon their OTC hearing aid capabilities. Curious to learn more? Check out Pros and cons of using Apple AirPods as hearing aids Things to consider when buying an OTC hearing aidThe HLAA recommends these questions to ask when buying an OTC hearing aid:
"Pay close attention to the return policy. In case OTC hearing aids don’t work out, you’ll want to know the process for returning them," recommends Michigan audiologist Amy Sarow. "Also, is there any person you can reach out to for support or questions? Some manufacturers have a phone number you can call or other options for support. It’s good to know your options in case you need them." And, be patient. "Getting used to hearing aids can take weeks, so be sure to give your brain the time to get used the amplification and hearing sounds differently," Sterkens says. To make sure you're only considering legitimate OTC hearing aid options, check out our piece on how to spot an OTC hearing aid scam. Additional FAQsHow do I know if I have mild or moderate hearing loss?The best way to know if you have the type of hearing loss that could benefit from OTC devices is to have a professional hearing test. However, it can also be helpful to know some key signs of mild or moderate hearing loss such as:
Learn about these and other early warning signs of hearing loss. Do OTC hearing aids help with tinnitus?While hearing aids can offer relief for many with tinnitus, OTC hearing aids probably won't offer as much benefit as prescription models. Hearing aids that are professionally fitted often have tinnitus masking features and other tools, as well as ongoing audiological care, which can be essential for tinnitus management. More: Will OTC hearing aids help with tinnitus? Will audiologists make adjustments to OTC hearing aids?While some audiologists are open to fine-tuning or adjusting OTC devices, others are not. Similarly, some hearing care specialists might not make adjustments, but will provide guidance on selecting OTC options and discussing their benefits and potential limitations. It's best to ask in advance whether a specific provider offers assistance with OTC hearing aids. How to find the right hearing care provider for youWhile OTC hearing aids can be a good first step for some, it's important to talk to a hearing specialist to help you find the right solution and ensure you get the most benefit from your hearing care. If you're ready to take action, browse our directory of hearing aid clinics near you to make an appointment. Emily Ostrowski, content manager, Healthy Hearing
|
Featured clinics near me
Earzlink Hearing Care - Reynoldsburg
7668 Slate Ridge Blvd
Reynoldsburg, OH 43068

Find a clinic
Need a hearing test but not sure which clinic to choose?
Call 1-877-872-7165 for help setting up a hearing test appointment.


 Emily is an experienced journalist and medical content writer based in Maine. Passionate about delivering enlightening and accurate content, she is committed to empowering people to make informed choices regarding their hearing health.
Emily is an experienced journalist and medical content writer based in Maine. Passionate about delivering enlightening and accurate content, she is committed to empowering people to make informed choices regarding their hearing health.